eLearning Self-paced
Understanding Inflammatory Bowel Disease
Overview
Guide to Study
eLearning Activity
When discussing IBD, it is important to also discuss IBS (Irritable Bowel Syndrome) and contrast both disorders. Inflammatory Bowel Disease (IBD) is a broad term that refers to chronic swelling and inflammation of the intestines. It's often confused with the non-inflammatory condition,irritable bowel syndrome (IBS). Although the two disorders share similar names and some of the same symptoms, they have distinct differences.
Different intestinal disorders can produce similar symptoms. Irritable bowel syndrome is a condition that produces some symptoms similar to those of Inflammatory Bowel Disease, but they are not the same condition, and they involve very different treatments. Therefore, getting an accurate diagnosis is essential to managing a patient’s condition properly. Here is a quick review of IBS and how it differs from IBD.
Irritable bowel syndrome is classified as a functional gastrointestinal disorder, which means there is some type of disturbance in bowel function. It is not a disease, but rather a syndrome, defined as a group of symptoms. These typically include chronic abdominal pain or discomfort and diarrhea, constipation, or alternating bouts of the two. People with IBS are also more likely to have other functional disorders such as fibromyalgia, chronic fatigue syndrome, chronic pelvic pain, and temporomandibular joint (TMJ) disorder.
IBS does not cause inflammation. IBS does not produce destructive inflammation. IBS seldom requires hospitalization, and treatment does not usually involve surgery or powerful medications, such as steroids or immunosuppressives. IBD is inflammatory, destructive, and treatments often include hospitalizations with surgeries and very powerful medications.
Now let’s talk more about IBD and its subtypes, Crohn's and Ulcerative Colitis.
The small bowel, also known as the small intestine, connects the stomach to the large intestine. The small bowel performs many functions including food digestion and absorption of essential nutrients from food into the body. Common conditions within the small bowel include Crohn's Disease, iron deficiency anemia (IDA) and obscure gastrointestinal bleeding (OGIB). Inflammation, lesions, ulcers and bleeding impair the digestion process and disturb normal absorption of nutrients, resulting in various symptoms.
Inflammatory Bowel Disease (IBD) affects an estimated 1.6 million Americans with 70,000 new cases diagnosed each year. Most patients are diagnosed before 35 years of age. A second occurrence of disease occurs in patients in the age range of 50 to 65 years. These chronic diseases tend to run in families and they affect males and females equally. While IBD can affect anyone, Caucasians are more likely than other ethnic groups (such as Ashkenazi Jewish populations) to have IBD.
IBD involves chronic inflammation of the digestive tract. Crohn’s and Ulcerative Colitis are the major conditions within this IBD umbrella. There are two main subtypes of IBD: Crohn's Disease, which can involve all parts of the gastrointestinal tract, even extraintestinal manifestations, and is patchy in its appearance and Ulcerative Colitis, which is isolated to the colon alone.
Both Crohn's Disease and Ulcerative Colitis usually involve severe diarrhea, pain, chronic abdominal pain, and fatigue and weight loss. Both of these conditions can be debilitating and sometimes lead to life-threatening complications. Due to the similar symptom profiles, it is critical to confirm the appropriate diagnosis, as treatment options may vary.
Crohn's Disease is a chronic condition that causes inflammation of the lining of the digestive tract. The inflammation often spreads deep into affected tissues and can affect the entire thickness of the bowel wall, as depicted in the following graphic.
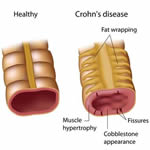
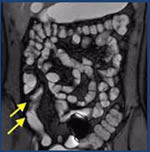
In Crohn’s Disease, inflammation can involve different areas of the digestive tract — anywhere from mouth to anus, although it is predominantly found in the small bowel. The inflammation of the intestine can “skip,” leaving normal areas in between patches of diseased intestine. The longer someone has Crohn's Disease, the more likely they will be impacted by penetrating disease, which can lead to strictures, obstructions and/or fistulas in the intestines.
What Causes Crohn's Disease?
The exact cause of Crohn's Disease is unknown. Researchers believe the following factors may play a role in causing Crohn's Disease:
- Autoimmune reaction
- Genes
- Environment
The Autoimmune reaction: Scientists believe one cause of Crohn's Disease may be an autoimmune reaction—when a person's immune system attacks healthy cells in the body by mistake. Normally, the immune system protects the body from infection by identifying and destroying bacteria, viruses, and other potentially harmful foreign substances. Researchers believe bacteria or viruses can mistakenly trigger the immune system to attack the inner lining of the intestines. This immune system response causes the inflammation, leading to symptoms.
Genes: Crohn's Disease sometimes runs in families. Research has shown that people who have a parent or sibling with Crohn's Disease may be more likely to develop the disease. Researchers continue to study the link between genes and Crohn's Disease.
Environment: Some studies suggest that certain things in the environment may increase the chance of a person getting Crohn's Disease, although the overall chance is low. Nonsteroidal anti-inflammatory drugs, antibiotics, and oral contraceptives may slightly increase the chance of developing Crohn's Disease. A high-fat diet may also slightly increase the chance of getting Crohn's Disease.
Some people incorrectly believe that eating certain foods, stress, or emotional distress can cause Crohn's Disease. Emotional distress and eating certain foods do not cause Crohn's Disease. Sometimes the stress of living with Crohn's Disease can make symptoms worse. Also, some people may find that certain foods can trigger or worsen their symptoms.
Who is at risk for Crohn's Disease? Crohn's Disease can occur in people of any age. However, it is more likely to develop in people between the ages of 20 and 29 who have a family member (most often a sibling or parent) with IBD who smoke cigarettes. It takes an average of 3 years from the onset of symptoms until diagnosis, and in some cases, it may take even longer.
People suffering from Crohn’s often experience chronic diarrhea, chronic abdominal pain and weight loss, which may be due to chronic diarrhea or fear of consuming food with severe symptoms. A feeling of low energy and fatigue is also common for these patients, which may be a result of anemia. Among younger children, Crohn's Disease may delay growth and development, and cause a failure to thrive. Crohn's Disease is a chronic disease, so this means patients will likely experience periods when the disease flares up and causes symptoms, followed by periods of remission when patients may not notice symptoms at all.
In severe cases, Crohn's Disease can lead to tears (fissures) in the lining of the anus, which may cause pain and bleeding, especially during bowel movements. Inflammation may also cause a fistula to develop. A fistula is a tunnel that leads from one loop of intestine to another, or that connects the intestine to the bladder, vagina, or skin. This is a serious condition that requires immediate medical attention. Symptoms of inflammation can occur outside of the intestines and include joint pain or soreness, eye irritation and skin changes that involve red, tender bumps under the skin.
Crohn's Disease is difficult and challenging to diagnose and manage, because every patient’s condition is different; the symptoms, onset, extent and severity of the disease will vary. Patient symptoms don’t always correlate with disease severity. On average, it takes 36 months and approximately 4.5 procedures for a patient to be diagnosed with Crohn's Disease.
It is critical to get an early diagnosis for these patients, because the longer the disease impacts the bowel, the more penetrating the disease becomes, and the higher the risk of further health concerns.
Studies also show that the more proximal the disease is found, the more severe the disease becomes and can be a leading indicator of relapse.
It is important to understand the physician’s decision-making process with these patients, and what test helps their diagnosis and treatment plan. Initial testing includes gathering the patient’s medical and family history, doing a physical exam, running lab tests, conducting radiologic examinations (CTE, MRE, SBFT) and doing an intestinal endoscopy. Many studies have shown that capsule endoscopy is a valuable adjunctive diagnostic test after conventional endoscopy and ileocolonoscopy. Crohn’s Video Capsule, a video capsule endoscopy specifically designed for patients suspected of having Crohn’s disease, can provide the physician with a more complete assessment of the location, extent, and severity of disease. Early diagnosis can lead to early treatment which may improve patient outcomes. Additionally, early onset of the disease may result in subtle flat lesions in the small bowel that many other tests may not be able to identify.
Although 30-35% of Crohn's patients have disease in the small bowel alone, the disease can develop in different areas of the GI tract. Disease activity and severity can vary widely over time and most patients have active disease at the time Crohn's Disease is diagnosed.
Traditional endoscopic tests cannot reach the deeper small bowel and other adjunctive tools, such as capsule endoscopy, are needed. There are 20 feet of small intestine not visualized by an endoscope.
We will delve more into diagnostic tests later in the module.
There is no cure for Crohn’s disease. Medical and surgical therapies are palliative and aimed at relieving acute exacerbations or complications. Dietary therapies aim to replenish depleted nutrient stores, allow for intestinal protein synthesis and healing, and offer pre-op preparation. Therapeutic measures may include diet, medications, surgery and psychological support (SGNA,2019).
Since Crohn's Disease impacts different areas of the bowel and may be more severe in some areas, treatment options may change over time. There are five main categories of medications used to treat Crohn’s Disease:
- Aminosalicylates are given orally or rectally and act to decrease inflammation at the wall of the intestine. Examples: Mesalamine, Balsalazide, Olsalazine, Sulfasalazine
- Corticosteroids affect the body’s ability to begin and maintain an inflammatory process. They are effective for short-term control of flare-ups but are not recommended for long-term or maintenance use because of their side effects. Examples: Glucocorticoids, Prednisone
- Immunomodulators are a class of medication that modifies the activity of the immune system so that it cannot cause ongoing inflammation. Examples: Cyclosporine, Azathioprine, 6-MP, Methotrexate
- Antibiotics may be used for Crohn's Disease when it impacts the colon or the area around the anus.
- Biologic therapies are indicated for people with moderately to severely active disease who have not responded well to conventional therapy. Examples: TNF ACE inhibitors, Infliximab (IV), Adalimumab, Certolizumab, Adhesion molecule inhibitor, Natalizumab
The approach to treatment for Crohn's Disease must be tailored to the individual. Factors that determine the approach to treatment include: disease severity, anatomic location of disease, previous response to medication, side effects of medication and/or comorbidities, other diseases and medical conditions.
Physicians will approach the management of Crohn's Disease, based on their own experiences. Approaches vary across gastroenterologists.
Top down approach: More aggressive drugs such as biologics are used early to reduce the opportunity of progression to a penetrating fistulizing disease.
Bottom up approach: Starts with less aggressive therapy to treat symptoms, moving to stronger drugs when current therapy is no longer effective.
These medications may not adequately control symptoms for everyone with IBD, and some people with these conditions develop complications that require surgery. According to the Crohn’s & Colitis Foundation of America (CCFA), about 70% of people with Crohn's Disease eventually require surgery.
The CCFA goes on to say with medical and/or surgical treatment:
- About 50% of patients will be in remission or have mild disease over the next five years
- 45% of those in remission will remain relapse-free over the next year
- 35% will have one or two relapses
- 11% will have chronically active disease
With a confirmation of an accurate diagnosis the ultimate goal is to:
- Induce remission which is defined as the absence of inflammatory symptoms with the goal of mucosal healing.
- Maintain remission:
- 95% of patients require maintenance therapies
- Transition to maintenance occurs after successful induction
- Need effective and safe long-term therapies
- Avoid complications of the disease and of the therapy
- Enhance the quality of life
Since the goals of the physician are to reduce symptoms, decrease hospitalizations, reduce the need for surgery, and to improve the patient’s overall quality of life, the patient should be monitored to determine if treatments are working.
Ulcerative Colitis is a chronic disease of the large intestine, also known as the colon, in which the lining of the colon becomes inflamed and develops tiny open sores, or ulcers, that produce pus and mucus. The combination of inflammation and ulceration can cause abdominal discomfort and frequent emptying of the colon.
Ulcerative Colitis and Crohn's are so similar in symptoms, that a term of Indeterminate Colitis (IC) has also been coined as a subgroup of IBD. Indeterminate colitis originally referred to those 10 to 15% of cases of Inflammatory Bowel Disease (IBD) in which there was difficulty distinguishing between Ulcerative Colitis and Crohn's Disease in the biopsy.
Most cases of Indeterminate Colitis eventually evolve into definite Crohn's Disease or Ulcerative Colitis, but a percentage of patients remain with a diagnosis of IC for many years without ever showing typical features of either disease, suggesting that IC might represent a separate subgroup of IBD. Capsule endoscopy can help reclassify IC to Crohn's Disease as cited by Cohen el al in the 2008 publication Journal of Pediatric Gastroenterology and Nutrition.
Because Crohn's and UC are so closely similar in symptoms it is important to make the distinction between the two, especially as the doctor evaluates the patient for treatment options. The management and treatment for these two different diagnoses will vary, so it is important to differentiate Crohn's Disease from Ulcerative Colitis. Crohn's Disease can affect any part of the Gastrointestinal (GI) Tract, but Ulcerative Colitis affects only the colon. Additionally, while Crohn's Disease can affect all layers of the bowel wall, Ulcerative Colitis only affects the lining of the colon.
| Crohn’s Disease | Ulcerative Colitis | |
|---|---|---|
| Location | Mouth to anus involvement | Colon only |
| Inflammation Pattern | Patchy | Continuous |
| Inflammation Level | Full-thickness | Superficial |
| Involvement | Variable | Variable |
| Extra-intestinal Manifestations | Yes | Yes |
| Strictures | Yes | Yes |
| Fistulae | Yes | No |
| Increased Colorectal Cancer risk | Yes, if colon involvement with longstanding colitis | Yes |
Although considerable progress has been made in IBD research, investigators do not yet know what causes this disease. Studies indicate that the inflammation in IBD involves a complex interaction of factors: genetics, the immune system and environmental factors. Foreign substances (antigens) in the environment may be the direct cause of the inflammation, or they may stimulate the body's defenses to produce an inflammation that continues without control.
Ulcerative Colitis may affect as many as 700,000 Americans. Men and women are equally likely to be affected, and most people are diagnosed in their mid-30s. The disease can occur at any age and older men are more likely to be diagnosed than older women.
While Ulcerative Colitis tends to run in families, researchers have been unable to establish a clear pattern of inheritance. Studies show that up to 20 percent of people with Ulcerative Colitis will also have a close relative with the disease.
About half of all patients with Ulcerative Colitis experience mild symptoms:
- bowel movements become looser and more urgent
- persistent diarrhea
- chronic abdominal pain
- bloody stools
- stool is generally bloody
- crampy abdominal pain
- weight loss
- low energy levels/fatigue
Among younger children, Ulcerative Colitis may delay growth and development. This is also true for Crohn's Disease as well; in fact, failure to thrive is a trigger for testing.
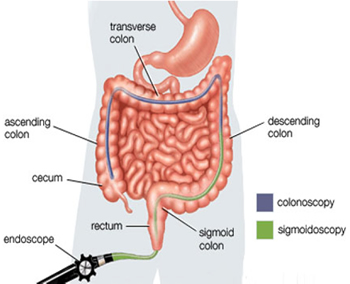
The physician will make a diagnosis based on medical history, a physical examination and a series of tests. The first goal of these tests is to differentiate Ulcerative Colitis from infectious causes of diarrhea. The physician will conduct a physical exam and interview the patient to learn more about their general health, diet, family history and environment. Blood and stool samples will be obtained. Stool specimens are analyzed to eliminate the possibility of bacterial, viral, or parasitic causes of diarrhea. Blood tests can check for signs of infection as well as for anemia, which may indicate bleeding in the colon or rectum. Following this, the patient generally undergoes an evaluation of the colon, using one of two tests -- a sigmoidoscopy or colonoscopy with biopsies.
Sigmoidoscopy/Colonoscopy involves the insertion of a scope into the rectum and lower colon to allow visualization to determine the extent and degree of inflammation in these areas. A colonoscopy may be utilized to look for any polyps or pre-cancerous changes in the setting of colitis. Chromoendoscopy is a technique of spraying a blue liquid dye during the colonoscopy in order to increase the ability of the endoscopist to detect slight changes in the lining of the intestine. The technique may identify early or flat polyps which can be biopsied or removed.
Since Crohn's Disease is patchy in nature and can affect any portion of the bowel, many physicians will try to evaluate the terminal ileum to ensure disease isn’t in the small bowel before making a diagnosis of Ulcerative Colitis. If an ileocolonoscopy is negative, some literature suggests that further evaluation of the small bowel be investigated to rule out Crohn's Disease due to similarities of both IBD sub-types. We will delve more into diagnostic tests later in the module.
The treatment for Ulcerative Colitis, as well as Crohn’s Disease and other IBD conditions, is multifaceted and includes the use of medication, alterations in diet and nutrition, and sometimes surgical procedures to repair or remove affected portions of the GI tract. Medication for Ulcerative Colitis can suppress the inflammation of the colon and allow for tissues to heal. Diarrhea, bleeding, and abdominal pain can be reduced and controlled with effective medication.
In addition to controlling and suppressing symptoms (inducing remission), medication can also be used to decrease the frequency of symptom flare-ups (maintaining remission). With proper treatment over time, periods of remission can be extended, and periods of symptom flare-up can be reduced.
There are five major classes of medication that are used today to treat Ulcerative Colitis:
- Aminosalicylates are given orally or rectally and act to decrease inflammation at the wall of the intestine.
- Corticosteroids affect the body’s ability to begin and maintain an inflammatory process. They are effective for short‐term control of flare-ups but are not recommended for long‐term or maintenance use because of their side effects.
- Immunomodulators are a class of medication that modifies the activity of the immune system so that it cannot cause ongoing inflammation.
- Antibiotics may be used for Ulcerative Colitis when it impacts the colon or the area around the anus.
- Biologic therapies are indicated for people with moderately to severely active disease who have not responded well to conventional therapy.
In some circumstances, a health care provider may recommend adding an additional therapy that will work in combination with the initial therapy to increase its effectiveness. For example, combination therapy could include the addition of a biologic to an immunomodulator. As with all therapy, there are risks and benefits of combination therapy. Combining therapies can increase the effectiveness of IBD treatment, but there may also be an increased risk of additional side effects and toxicity.
With Ulcerative Colitis, one-quarter to one-third of patients may not respond to medical therapy or they may experience complications. Under these circumstances, surgery may be considered. Surgery involves the removal of part of or the entire colon (colectomy).
Depending on a number of factors, including the extent of the disease and the patient's age and overall health, one of two surgical approaches may be recommended. The first involves the removal of the entire colon and rectum, with the creation of an ileostomy or external stoma (an opening on the abdomen through which wastes are emptied into a pouch, which is attached to the skin with adhesive).
Another option also calls for removal of the colon, but it avoids an ileostomy. By creating an internal pouch from the small bowel and attaching it to the anal sphincter muscle, the surgeon can preserve bowel integrity and eliminate the need for the patient to wear an external ostomy appliance.
With a confirmation of an accurate diagnosis, the ultimate goal in treating ulcerative colitis is to help patients regulate their immune system better and avoid complications of both the disease and the therapy. Remission, defined as the absence of inflammatory symptoms, can be achieved temporarily.
The symptoms of Ulcerative Colitis do tend to come and go, with fairly long periods in between flare-ups in which patients may experience no distress at all. These periods of remission can span months or even years, although symptoms do eventually return.
The jury is still out on mucosal healing as an endpoint, but clinical and symptomatic outcomes should be monitored.
It can be very challenging for a doctor to reach a definitive diagnosis. On average, it takes 36 months and approximately 4.5 procedures for a patient to be diagnosed with Inflammatory Bowel Disease. Early diagnosis is key for these patients, because the longer the disease impacts the bowel, the more penetrating the disease becomes, and the higher the risk of further health concerns. It is important for patients to ask for a definitive diagnosis and treatment plan.
Living with IBD has its challenges. Since it is a chronic disease, there are times when patients will feel fine and there are flare-ups where patients can become very sick. As someone taking care of these patients, it’s important to keep in mind what they are going through. Patients need to find the right physician for them. Since this will be a long road, they should find a physician with whom they are comfortable and confident about having a treatment plan in place. In addition, remind patients that they need to be patient. Medications can take some time to start working, and the first one may not be the right one. Flexibility is needed in the event that medications need to be adjusted over time. Patients must also learn to listen to their body. There will be times when they cannot keep up their usual busy schedule and they need to rest.
One of the most important things patients need to know is that it is critical to keep taking their medication, even if they feel fine, to prevent future flare-ups. If one stops their medication, it is possible that when they really need it, it may no longer work for them. Because symptoms do not correlate with disease activity, a lot of damage can be done to the intestines without realizing it.
Lastly, there are many organizations that offer a wealth of resources on IBD including up-to-date information and support groups where one can meet others who are going through the same journey. Some organizations to recommend include the Crohn’s & Colitis Foundation of America (CCFA) as well as www.YouandIBD.com
GI specialists have many resources at their disposal to diagnosis the appropriate IBD sub-type. The modalities that they may use for detecting and monitoring Crohn's Disease include sigmoidoscopy, colonoscopy, double-balloon enteroscopy, small bowel follow through, EGD, flexible sigmoidoscopy, MRE, CTE, capsule endoscopy and the Crohn’s Video Capsule.
The American Journal of Gastroenterology published in 2014 found that small bowel follow-through and CTE scans of the small bowel are valuable, however CTE exposes the patient to radiation and is less accurate for early disease detection in the small bowel.
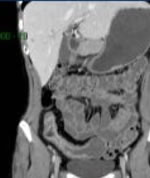
GI specialists have many resources at their disposal to diagnosis the appropriate IBD sub-type. CT enterography provides better visualization of the entire small bowel wall and shows extra-enteric complications of small bowel disease. If Crohn's Disease is suspected, capsule endoscopy can provide direct visualization of the small bowel mucosa (where other modalities don’t) and can assist in a more timely diagnosis.
Video capsule endoscopy would not be used alone for the diagnosis of IBD or Crohn's Disease, but it can provide an initial diagnosis with the use of inflammatory markers, GI or extraintestinal symptoms, and other imaging techniques. The use of video capsule provides an opportunity to treat and manage Crohn’s Disease, to verify therapy is working effectively.
The video capsule platform includes four different video capsules- each with technical differences, targeted anatomy and intended uses. The SB3 Capsule is intended for visualization of the small bowel. It is intended for visualization and detection of suspected pathology that may be related to obscure bleeding, iron deficiency anemia or Crohn’s disease. The Crohn’s Video Capsule, is intended for visualization of the small bowel and colonic mucosa.
The Crohn’s Video capsule is specifically designed to be used for patients suspected of having Crohn’s Disease. It is intended for visualization of the small bowel and colonic mucosa:
- It may be used in the visualization and monitoring of lesions in the small bowel that may indicate Crohn’s disease not detected by upper and lower endoscopy. It is also used for the visualization of inflammation of the colon in patients with colonoscopy-diagnosed Crohn’s disease
- It may be used in the visualization and monitoring in the small bowel of lesions that may be a source of obscure bleeding (either overt or occult) or that may be potential causes of iron deficiency anemia (IDA) not detected by initial upper and lower endoscopy
- The Crohn’s Video Capsule may be used as a tool in the detection of abnormalities of the small bowel
- The Crohn’s Video Capsule may be used as a tool in the detection of abnormalities of the small bowel; it is intended for use in adults
- The SB3 video capsule may be used in the visualization and monitoring of lesions that may indicate Crohn’s disease not detected by upper and lower endoscopy. It features the Suspected Blood Indicator (SBI), which is intended to mark frames of the video suspected of containing blood or reddened areas. It is intended for use in adults and children from 2 years of age.
Contraindications:
The video capsule is contraindicated for use under the following conditions:
- In patients with known or suspected gastrointestinal obstruction, strictures, or fistulas based on the clinical picture or pre-procedure testing and profile
- In patients with cardiac pacemakers or other implanted electromedical devices
- In patients with dysphagia or other swallowing disorders
- In patients with allergies or known contraindication to the medications and preparation agents used in the procedure as described in the relevant instructions for use
Procedure Risk Information
The risks of the video capsule include capsule retention, aspiration, and skin irritation. The risks associated with colon preparation are allergies or other known contraindications to any preparation agents or medications used for the video capsule system regimen, according to laxative medication labeling and per physician discretion. Medical, endoscopic, or surgical intervention may be necessary to address any of these complications, should they occur. After ingesting the video capsule, and until the capsule is excreted, patients should not be near any source of powerful electromagnetic fields, such as one created near an MRI device.
As physicians strive to make a diagnosis, many tools, including the video capsule endoscopy, can assist physicians with the medical management of their disease. Several of the following studies prove that VCE for Crohn’s disease is invaluable in diagnosing and managing the disease.
A study in Clinical Gastrointestinal and Hepatology showed that capsule endoscopy had a higher sensitivity and specificity as compared to CTE for diagnosing Crohn's Disease. Additionally, this study shows higher yield of diagnostic findings in the proximal small bowel with capsule endoscopy than using radiologic examination. The study evaluated 93 patients, comparing the accuracy of capsule endoscopy in patients with newly diagnosed Crohn’s Disease.
| Method | Sensitivity | Specificity |
|---|---|---|
| CE | 100% | 91% |
| CTE | 76% | 85% |
| MRE | 81% | 86% |
A study by Ben-Horit,et al. demonstrated that longitudinal VCE- based monitoring of patients with quiescent Crohn’s disease is practical, safe and could be considered as part of the monitoring options for Crohn’s disease patients.
In Italy, 18 patients with suspected or known Crohn’s Disease, were assessed by CE with the Crohn’s Video Capsule. In the suspected CD group, approximately one-half of patients had major inflammatory lesions, most of them being in the third tertile (distal portion of the small intestine). In 75% of these patients, the diagnosis was confirmed. In the established CD group, 90% of patients had significant lesions in the terminal and neoterminal ileum. No adverse events were reported. Another study done in Israel included 49 patients who were examined by the Crohn's Video Capsule in order to assess the system’s capacity to visualize and examine the small bowel and the colon. From 71% of patients who had established CD, 31% of them had proximal inflammatory lesions. All recordings were of good quality, and no retention of the capsule was reported.
Other Modalities
SBFT: The small-bowel follow-through (SBFT) examination has historically been the standard radiologic approach used to assess patients with active Crohn's Disease (CD), as more than 70% of patients have involvement of the small intestine. However, researchers in some studies have shown that SBFT is not accurate for detection of active CD in the small bowel. It has been suggested that small-bowel enteroclysis is more accurate than SBFT at detecting early mucosal lesions, but both methods provide only limited and indirect information in regard to the state of the bowel wall and extraluminal extension of CD.

CTE: computed tomographic (CT) enterography has become accepted as a noninvasive imaging technique to evaluate CD. In addition to allowing visualization of extraenteric structures, CT enterography with the use of oral neutral contrast agents and rapid intravenous contrast infusion can be used to reliably identify active inflammation in the small intestine. However, because patients with CD are often young and CD is a chronic and relapsing disease, they may undergo repeated imaging examinations to assess the status of their disease, which exposes them to radiation.
MRE: magnetic resonance (MR) enterography has been introduced as a radiation-free alternative method to evaluate patients with CD. Investigators in several reports have shown MR enterography to be useful for the identification of active ileitis, assessment of disease activity, and evaluation of extraenteric complications in patients with CD.
The sensitivity values of CT enterography and MR enterography for the detection of extraenteric complications have shown to be significantly higher than those for SBFT.
According to the 2015 ASGE guidelines, the authors concluded that capsule endoscopy is useful in the initial diagnosis of Crohn's Disease, for those who have no obstructive symptoms. The authors recommend patency capsule of radiology for those patients with suspicion of an obstruction before a capsule endoscopy procedure. The authors also recommended capsule endoscopy in patients with established Crohn's Disease and unexplained symptoms when abnormalities detected will alter management.
The small bowel performs many functions, including food digestion and absorption of essential nutrients from food into the body. Common conditions within the small bowel include the IBD subtypes, Crohn's Disease, and Ulcerative Colitis. These conditions cause inflammation, lesions, ulcers and bleeding that impair the digestion process and disturb normal absorption of nutrients, resulting in various symptoms.
In this program you learned specifically about the differences in the IBD subtypes, Crohn's Disease and Ulcerative Colitis. Both conditions usually involve severe diarrhea, pain, fatigue and weight loss. IBD can be debilitating and sometimes leads to life-threatening complications. When it comes to IBD, getting an accurate diagnosis can be a challenge. A combination of tests is used to confirm a diagnosis and to understand the extent and location of disease, which helps determine appropriate treatment options for affected patients.
CNE Certificate Process
Note: Your computer should be connected to a printer before completing the Post-Testing in order to permit printing your course certificate.